What is Glaucoma?
Glaucoma is a serious, lifelong eye disease that can lead to vision loss if not controlled. But for most people, glaucoma does not have to lead to blindness. That is because glaucoma is controllable with modern treatment, and there are many choices to help keep glaucoma from further damaging your eyes. Treatment cannot reverse damage that has already occurred, but it can prevent further vision loss. Glaucoma is an eye disease that causes loss of sight by damaging a part of the eye called the optic nerve. This nerve sends information from your eyes to your brain. When glaucoma damages your optic nerve, you begin to lose patches of vision, usually side vision (peripheral vision).


Types of Glaucoma
There are many types of glaucoma. Often, the cause of high pressure in the eye can help tell the type of glaucoma and the best treatment for it. The most common types include:
Chronic (Open Angle) Glaucoma
This is the most common type. In open angle glaucoma, aqueous fluid drains too slowly and pressure inside the eye builds up. It usually results from aging of the drainage channel, which doesn’t work as well over time. However, younger people can also get this type of glaucoma.
Normal Tension Glaucoma
This is a form of open angle glaucoma not related to high pressure. People with normal tension glaucoma may be unusually sensitive to normal levels of pressure. Reduced blood supply to the optic nerve may also play a role in normal tension glaucoma.
Acute (Angle Closure) Glaucoma
Those of Asian and Native American descent are at higher risk for this form of glaucoma. It occurs when the drainage system of the eye becomes blocked. It causes a sudden rise in pressure, requiring immediate, emergency medical care. The signs are usually serious and may include blurred vision, severe headaches, eye pain, nausea, vomiting or seeing rainbow-like halos around lights. Occasionally, the condition may be without symptoms; similar to open angle.
Secondary Glaucoma
Secondary glaucoma is the result of another eye condition or disease, such as inflammation, trauma, or tumor. Learn more about uveitis, an inflammation that can cause secondary glaucoma.
How Does Glaucoma Damage Your Eyes?
Doctors don’t know exactly how glaucoma damages the optic nerve. For many people, increased eye pressure seems to play an important role.
Your eye produces a watery fluid (aqueous humor), which goes into the eye and drains out. When your eye is healthy, the fluid drains through a mesh-like pathway and into the bloodstream. Aqueous fluid is produced by the ciliary body. It flows through the pupil and behind the clear cornea. Finally, it drains away through the trabecular meshwork.
For some people, fluid can’t drain properly because of a faulty drainage system. Drainage that once worked well may gradually slow down as you get older. A sink that becomes clogged backs up with water. When there is no place for excess fluid to go, pressure inside the eye builds up.
This increased eye pressure may damage the optic nerve over time. Slowly, the nerve fibers that are essential for vision die.
For others, glaucoma damages the optic nerve without increased pressure. These people may be unusually sensitive even to normal levels of pressure. Their glaucoma may also be related to problems with blood flow in the eye. Doctors continue to study eye pressure and other possible causes of glaucoma.
Different people experience glaucoma differently. Usually, glaucoma affects side vision (peripheral vision) first. Late in the disease, glaucoma may cause “tunnel vision.” In this condition, the person can only see straight ahead. That’s why someone with glaucoma can have good straight ahead (central) vision. However, even central vision can be seriously damaged.
Glaucoma Risk Factors
These risk factors may increase your chance of having glaucoma:
Age
The older you are, the greater you are at risk (especially if you are over 60 years old). African Americans are at a greater risk at a younger age starting at age 40 and older.
Race
African-Americans age 40 and over are 4-5 times more likely to have glaucoma than others. Hispanics are also at increased risk for glaucoma as they age. Those of Asian and Native American descent are at increased risk for angle closure glaucoma.
Family History
If you have a parent, brother or sister with glaucoma, you are more likely to get glaucoma. If you have glaucoma, inform your family members to get complete eye exams.
Medical History
You are at risk if you have a history of high pressure in your eyes, previous eye injury, long term steroid use, or nearsightedness.
Take Our Adult Vision Risk Assessment!
This self-assessment will help you determine whether you are at risk for age-related eye disease.
Signs of Glaucoma
There are three major signs that a person may have glaucoma:
- Optic nerve damage
- Increased eye pressure (elevated intraocular pressure).
- Vision loss (visual field loss)
Dilated Eye Exam
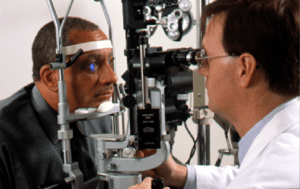
Credit: National Eye Institute, National Institutes of Health
Your eye doctor will check your eyes using some of these tests:
Ophthalmoscopy
The doctor will place a few drops in your eye to open or dilate the pupil. This allows the doctor a clearer view to inspect the optic nerve at the back of the eye.
Photography or Optic Nerve and Retinal Imaging
Photography or Optic Nerve and Retinal Imaging or laser scanning may be used to show the appearance of the optic nerve inside your eye. This may also involve dilating your eye.
Tonometry
Tonometry measures pressure in the eye. Medicine drops are used to numb the eye. An instrument gently presses on the outside of your eye. Pressure is shown as a number followed by the abbreviation “mm Hg.” This stands for “millimeters of mercury,” a standard measure for pressure. An average pressure is about 16 mm Hg. Still, a higher than average number doesn’t always mean you have glaucoma. Since the thickness of the cornea (the front window of the eye) may affect the pressure reading and the risk of glaucoma progression, your doctor may measure this as well. Pressure can also be measured by non-contact tonometry, also known as the air puff test.
Perimetry
Perimetry evaluates your visual field. This tests your vision all around your field of view to see if any areas are missing. It usually involves staring straight ahead at a light and trying to see lights that appear around the sides of your view. This is generally done with a computerized system.
Gonioscopy
Gonioscopy After numbing the eye, the doctor gently places a special lens on the surface to examine the area in the front of the eye that drains fluid. Gonioscopy allows a more accurate diagnosis of the type of glaucoma.
Take Our Adult Vision Risk Assessment
This self-assessment will help you determine whether you are at risk for age-related eye disease.
Glaucoma Treatment
Glaucoma can usually be treated and controlled using medicine(s), laser surgery, glaucoma surgery or a combination of these treatments. Medicines (eye drops) are typically the first step in treatment, but laser surgery may be just as effective as a first choice. Your treatment is up to you and your doctor. In this section, you will learn about your options for treatment.
Eye doctors use many medicines to treat glaucoma. These drugs lower pressure inside the eye. Often, people with glaucoma must take these medicines for life to control the pressure and limit vision loss.
An introduction to glaucoma medicines
Glaucoma medicines are usually in the form of drops, but also come in pills or ointment. They work to lower the amount of aqueous fluid produced and/or improve fluid drainage in the eye.
All glaucoma medicines may cause side effects, some of which can be uncomfortable. A few side effects can be quite serious, but those side effects are not common.
The glaucoma medicines listed below are grouped by the way they work. Some of the possible side effects are also listed. Not every drug in a category will have all the possible side effects listed. Your doctor can tell you which side effects are possible with the medicines you use. (NOTE: all glaucoma medicines may not be listed below.)
Prostaglandin Analogues
Prostaglandin Analogues are drugs that lower pressure in the eye by improving fluid drainage. They have the advantage of requiring use only once per day.
Possible side effects
A rare side effect may be a darkening of eye color. Often, there is an increased growth of eyelashes. Side effects can also include redness, itching, burning and blurred vision.
Medicine (Brand Name)
latanoprost (Xalatan®)
travoprost (Travatan®)
bimatoprost (Lumigan®)
unoprostone (Rescula®)
Beta-blockers
Beta-blockers decrease pressure inside the eye by reducing the amount of aqueous fluid your eye makes. These medicines are available as eye drops.
Possible side effects
These include possible respiratory problems, lowered heart rate and blood pressure, blurred vision, tiredness, forgetfulness, and changes in blood cholesterol levels. People with asthma, some kinds of heart disease or low blood pressure should be very careful about using beta-blockers to treat their glaucoma. Also, if a patient is on other “blocker” medicines for other health problems, the combined effect of the drugs could cause problems.
This is why it’s important to tell all of your doctors about all the medicines you are taking.
Medicine (Brand Name)
betaxolol (Betoptic®, Betoptic® S)
carteolol (Ocupress®)
levobunolol (Betagan®)
metipranolol (OptiPranolol®)
timolol hemihydrate (Betimol®)
timolol maleate (Timoptic®,Timoptic-XE®,Cosopt® (see also anhydrase inhibitors))
Alpha-adrenergic Agonists
Alpha-adrenergic agonists are eye drops that lessen the amount of aqueous fluid the eye makes and may also increase flow of fluid out of the eye. These drops are sometimes used after laser surgery to prevent sudden rises in pressure.
Possible side effects
These include allergic reactions, dry mouth, burning of the eyes, dilated pupils, nasal decongestion, and drowsiness.
Medicine (Brand Name)
apraclonidine (Iopidine®)
brimonidine tartrate (Alphagan®, Alphagan-P®)
Carbonic Anhydrase Inhibitors
Carbonic anhydrase inhibitors come in pills or drops. They reduce the amount of aqueous fluid the eye makes. Often, they are used when other drugs have not worked fully.
Possible side effects
The more common eye drop form of this drug may cause stinging, burning, a feeling of something in the eye, and an odd taste in the mouth. Taken as pills (only rarely nowadays), these drugs can have side effects throughout the body, including fatigue, tingling in the hands and feet, depression, frequent urination, anemia, kidney stones, loss of appetite, weight loss, diarrhea, and stomach cramps. Monitoring the dose of the oral pill and taking the medicine with food may help. Pregnant women and people sensitive to sulfa-related drugs should not take these medicines. A toxic reaction may occur if taken with large doses of aspirin. Very rarely, these drugs can lead to serious conditions known as Stevens-Johnson syndrome and aplastic anemia.
Medicine (Brand Name)
acetazolamide (Diamox®)
methazolamide (Neptazane®)
dichlorphenamide (Daranide®)
brinzolamide hydrochloride (Azopt®)
dorzolamide hydrochloride (Trusopt®, Cosopt®) – (see beta blockers)
Miotics
Miotics lower pressure by tightening tiny muscles inside the eye. This helps to open up the eye’s drainage system, making it easier for aqueous fluid to flow out of the eye. Miotics come in eye drops or gels. When used as drops, these drugs usually need to be used several times a day, increasing the chance of forgetting a dose. Miotics are not commonly used any more except in certain cases
Possible side effects
These include decreased pupil size, blurred vision, poor night vision, nearsightedness, watering eyes, brow and eye aches, and allergic reactions.
Medicine (Brand Name)
carbachol (Isopto® Carbachol)
pilocarpine (Isopto® Carpine, Pilocar®, Pilopine®, Pilagan®)
Other Medicines
Anticholinesterase Iodide
Medicine (Brand Name)
echothiophate iodide (Phospholine® Iodide)
Combinations containing two medicines in the same bottle
Cosopt® = Timoptic® and Trusopt®
E-pilo® = Epinephrine® and pilocarpine
Follow your treatment plan!
Follow Your Treatment Plan!
It’s up to you to follow your treatment plan and have regular follow-up visits. At follow-up visits, your doctor will check to see if your glaucoma is getting worse. Remember to report anything you believe may be a side effect of the medicine you are taking.
Don’t Skip Doses!
Take your medicine as scheduled. Skipping doses of your medicine may put your vision in danger and mislead your doctor. Be sure to tell your doctor if you’ve missed any doses.
With a chronic disease like glaucoma, it can be hard to remember to use medicines as directed. It may help to link taking medicine to the things you do every day like eating meals or brushing your teeth.
After evaluating your progress, your doctor may try changing your doses, switching medicines or changing other parts of your treatment to find the best results for you. Sometimes simple changes like adjusting your schedule to take your medicines at mealtimes or before bed can make your drug routine more comfortable.
Tips for Taking Your Glaucoma Medicine
- Ask your doctor to write down an exact schedule for taking your medicine, especially if you’re taking more than one.
- Ask your doctor what to do if you accidentally forget a dose. The instructions may be different depending on which medicines you are taking.
- Learn about the medicines you are taking and the best way to use them. Find out whether they need special handling, such as storing them in the refrigerator.
- If you take a combination of drops and ointments, always apply the drops first.
- Schedule your doses around your normal routine, such as when you wake up, when you eat meals, and when you go to bed at night.
- Keep your medicines in plain sight; it’s easier to remember to take them.
- Keep medicines in a clean place. For example, if you carry them in your purse, put them in a ziplock bag to keep them clean.
- Take your medicines with you when you’re away from home. If you’re checking luggage at the airport, keep your medicines with you in your carry-on or in your purse.
- If you forget a dose, do not automatically double your next dose. Instead, follow your doctor’s instructions on what to do.
- If you can’t remember whether you took your medicines, simply use one dose at your next scheduled time.
- Tell all of your doctors about all the medicines you are taking. Glaucoma medicines may interact with drugs prescribed for other conditions.
- Call your eye doctor if you notice any unusual changes in your eyes, your vision or the way you feel in general.
- Schedule regular checkups and follow through with them.
- Take care of yourself—your eyes and the rest of you along with them!
Taking Eye Drop Medications
A simple technique can keep more medicine in your eye and make glaucoma medication more effective.
Laser Surgery
Some people may need eye surgery to control their glaucoma. Lasers are very useful for treating glaucoma because they avoid cutting and have a lower chance of complications (compared to glaucoma surgery).
There are three common laser procedures:
Laser trabeculoplasty
Laser trabeculoplasty or selective laser trabeculoplasty improves the outflow of aqueous fluid. A laser is used to make from 50 to 100 tiny burns in the trabecular meshwork. The procedure opens up the mesh-like outflow pathway to improve draining of fluids from the eye. Sometimes your doctor may perform this procedure over two visits. The benefit of the treatment may last for a few years, but it is not a cure. More than half the people who have this surgery need additional treatment within five years. Repeat laser trabeculoplasty may be used to treat patients who had a good first effect with laser treatment, but over time have lost some of the pressure-lowering response. Treatment beyond a second laser treatment is most often not effective.
Peripheral iridotomy
A peripheral iridotomy is most often used to treat narrow angle or angle closure glaucoma. The laser beam creates a tiny hole in the colored part of the eye (the iris). This lets the pressure in front of the iris become the same as the pressure behind the iris. As a result, the iris moves away from the drainage angle and the aqueous fluid can resume draining normally.
People usually don’t feel any pain with these procedures, although some report a slight stinging. Most patients take it easy the day of their treatment, but go back to their normal routine the following day.
Many people need to keep taking medicines even after laser surgery.
Laser surgery is usually successful, but there are some risks. These include a temporary, generally short-term increase in eye pressure, temporary inflammation of the eye, and possibly a slightly increased risk of developing cataracts.
Is it Necessary?
If medicine or laser surgery does not relieve eye pressure, a patient may need glaucoma surgery. There are several options.
Filtering Surgery
Filtering surgery creates a new path through the eye’s tissues to let fluid drain from the eye.
In the most common filtering surgery, called a trabeculectomy or a sclerostomy, the surgeon makes a small opening in the white part of the eye (the sclera) to create a new outflow path. The fluid then flows through the new opening and creates a bleb, which is like a small bubble or reservoir on the surface of the eye. The bleb holds the fluid while it is slowly absorbed into the surrounding tissue. The upper eyelid usually hides the bleb, so it’s not noticeable to you or others.
Most people who have this procedure no longer need medicine after surgery. Some people treated still need medicine, but they have better pressure control after the surgery. About 15 percent do not benefit from filtering surgery.
An alternative type of glaucoma surgery may occasionally be performed in which the tissues over the drainage area are thinned but not fully penetrated. This procedure may produce fewer complicatons than trabeculectomy, but also may be less effective in achieving low intraocular pressures.
Drainage Implant Surgery
Drainage implant surgery is sometimes performed when a person is not suited for filtering surgery or when earlier filtering surgery has failed. Depending on the kind of implant used, the surgery is called valve, shunt or seton surgery.
In these procedures, the surgeon inserts a tiny tube through the sclera into the front part of the eye behind the iris. This tube becomes a path for fluid to drain away. The other end of the tube is attached to a tiny reservoir that acts like the bleb to hold fluid until it is absorbed into the surrounding tissue. The reservoir is placed on the surface of the eye, back between the eye muscles, so it is not visible.
Right after filtering or drainage implant surgery, a person may have a temporary decrease of vision. Vision usually improves over several weeks to its previous level. It also takes time to recuperate from either form of surgery. For example, in the weeks after surgery, people often must avoid getting water into their eyes, reading, bending, lifting heavy objects and driving.
Canaloplasty
Canaloplasty is a newer procedure to lower pressure that is performed within the eye wall but that does not actually pentrate the eye. While this procedure is safer that filtering surgery, it does not provide as profound a reduction in IOP.
Minimal Invasive Glaucoma Surgeries
Minimal Invasive Glaucoma Surgeries are a set of newer FDA approved procedures that lower pressure. These approaches currently include Trabectome and the iStent. Both of these approaches work by bypassing the blockage in the drain of the eye to help fluid flow through the natural drain and do not require “artifical” pathways for fluid drainage to areas outside the eye. Like canaloplasty, the procedures are less risky than filtering surgery but do not provide as profound a reduction in IOP. More long-term data is needed to determine how well they work beyond the first few years. Use of Minimal Invasive Glaucoma Surgeries is still being debated among glaucoma specialists but may have application is specific patients.
Laser Cyclophotocoagulation
Laser Cyclophotocoagulation is used for severe cases of glaucoma. It eliminates tiny areas of the ciliary body that make aqueous fluid. This “turns down the faucet.” Laser cyclophotocoagulation requires a numbing block to the eye to prevent pain with the procedure
Risks of Glaucoma Surgery
Glaucoma surgeries have some possible risks, such as:
- A higher chance of getting cataracts
- Infection or leaking of the incision
- Too low pressure
- Hemorrhages inside the eye
Unfortunately, the new drainage path can close, causing pressure in the eye to rise again. Filtering surgery can be repeated with good results. Also, drainage implants are often successful in patients whose filtering surgery has failed. The medicines that reduce inflammation and control scar formation after surgery have helped increase the success of glaucoma surgeries.
Glaucoma Treatment
You must work with your eye doctor if you have glaucoma. Eye doctors know how to treat glaucoma, but they have to work with you to find the best way to treat your disease.
What You Do Makes a Difference
- Remember to take notes. Write down your questions
so you can make the most of your eye doctor visits. - Explain to your eye doctor how the medicines you are taking affect you.
- Tell all of your other doctors about your eye medicines and all other drugs you’re taking.
- Read more about glaucoma and how to live with it.
- Tell the eye doctor about any changes in your physical condition, any changes in your medicine or any
side effects
Getting More Involved in Your Treatment
Even if surgery or drugs lower pressure in your eye, it’s still possible to lose vision. Therefore, you and your doctor must carefully monitor the disease.
Since you will be visiting your eye doctor regularly, take time and care in choosing a person who you are comfortable with. Your doctor should understand that your questions and concerns are important. A doctor who is willing to work with you, listen to your concerns and provide the best treatment, plays a large part in your success against glaucoma.

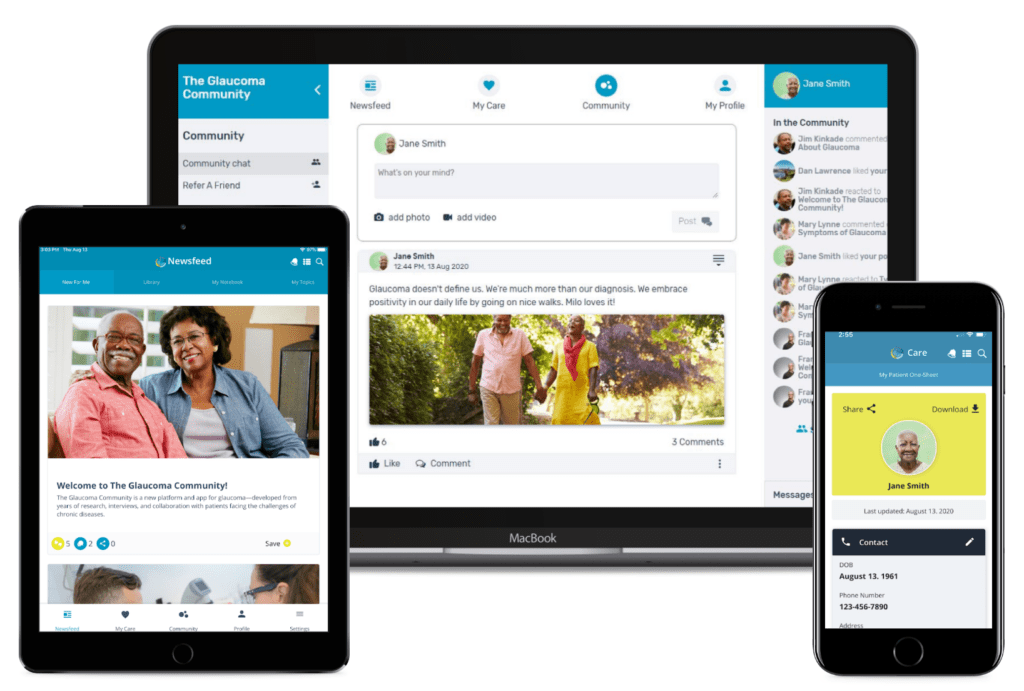
The Glaucoma Community provides a toolkit of useful, personalized features designed to meet the needs of patients and caregivers. Find out more at responsumhealth.com/glaucoma.
You have to help save your sight
You may need medicines every day for the rest of your life. Find support and encouragement from your family, friends and others. Sometimes it helps to talk to people who have experienced the same thing. It can help you to discuss side effects, share ways to remember your medicines and celebrate getting your glaucoma under control.
Unfortunately, there are a few people whose eyesight will continue to get worse, despite doing all the right things to control their glaucoma. Doctors aren’t sure why this happens, but research in this area continues.
The future holds great promise for treating glaucoma. New medicines are being developed. Other treatments may soon become available. In the meantime, take heart in knowing that you’re doing everything possible to treat your glaucoma successfully. The doctor/patient team approach, support from others and promising scientific discoveries will help you look forward to a bright future.
Questions for Your Eye Doctor
You will have many questions as your doctor diagnoses and treats your glaucoma. It’s helpful to keep a list of these questions, especially if they come to mind in between your eye appointments. Write all your questions down and bring the list with you, then discuss them with your doctor. Here are some questions many people have:
- What do these medicines do?
- How much will they cost? Will my insurance help pay
for them? (These may be questions for your insurance company, not your doctor.) - What are the possible side effects of my medicines?
- Can I do anything to lower the chance of side effects or reduce the effects?
- What should I do if I miss a dose?
- Will I need surgery? What are the benefits and drawbacks of laser surgery? Of glaucoma surgery?
- What will my vision be like after surgery?
- How long will recovery take? How will I need to change my usual activities? Will I be able to drive? Go to work?
- Would I still need medicine after surgery? The same doses?
- How often will I need return visits?
- What is the latest research on glaucoma and its treatment?
- Are there any other treatments that may be right for me at this stage of my disease?
A simple technique can help keep more medicine in your eye and make glaucoma medicines more effective.
Medicare Benefits and Your Eyes
The Welcome to Medicare Physical covers screening for glaucoma.
Glaucoma Financial Assistance Information
Contact information for organizations and services that may be able to help with the cost of vision care.
The Glaucoma Community
An online community that empowers people with glaucoma through knowledge, support, and shared experiences
Living Well with Low Vision is an online resource to educate those with loss of vision on how maintain their independence and quality of life. Learn more at lowvision.preventblindness.org.
![]()